Reaching 80% Before 2016: UW Health’s Journey


Dr. Jennifer Weiss, MD, MS, is an Assistant Professor in the Department of Medicine-Gastroenterology at University of Wisconsin-Madison. Her research focuses on colorectal cancer screening for both average-risk and high-risk populations. Dr. Weiss has served as a physician leader of the UW Health Colon Cancer Prevention Initiative, which developed and implemented multiple complex system-wide colorectal cancer screening interventions that assisted in increasing screening rates from 61% to 81% over the past six years. She has a five-year career development award from the American Cancer Society to identify patient, provider, and system barriers to colorectal cancer screening and optimize interventions that target these barriers. Dr. Weiss is also the Director of the UW Gastroenterology Genetics Clinic where she cares for patients at high-risk for developing colorectal cancer. Dr. Weiss recently presented on UW Health’s journey to reach an 80% screening rate at NCCRT’s 2015 Annual Meeting. We are thrilled to welcome her back to share her story with our readers.
Hi, Dr. Weiss! We’re happy to reconnect and to feature you on the 80% by 2018 Blog. Can you tell us a little about yourself and how you ended up working on systems changes to increase colorectal cancer screening?
During both my internal medicine training and my practice as a gastroenterologist, I have seen many patients diagnosed with a colorectal cancer (CRC) that could have been prevented with appropriate screening. CRC is preventable! I tell all my patients that the purpose of CRC screening is to identify and remove the pre-cancerous lesions (adenomas) and prevent progression to colorectal cancer. CRC screening is an amazing process, however, it is also complex with multiple steps and potential barriers. Many barriers exist at the level of the healthcare system (e.g. lack of capacity to perform screening exams, problems with easily identifying patients who are overdue for screening exams, and lack of a reliable follow-up process for ordered exams). I believe that if we can overcome these barriers, we can help save close to 50,000 lives each year.
Tell us a little bit about UW Health Clinics.
UW Health is one of the 12 largest multispecialty physician groups in the United States and provides 2.4 million outpatient visits per year. It is comprised of both multispecialty and community-based primary care clinics, with nearly 400 primary care providers in 50 primary care clinic sites across south central Wisconsin. The patient population we serve is approximately 90% white, 4% African American, 3% Hispanic or Latino, and 3% Asian or Pacific Islander. Approximately 70% have commercial insurance, 20% are covered by Medicare, and the remainder have Medicaid or are uninsured.
How did UW Health decide to focus on increasing colorectal cancer screening?
UW Health is a member of the Wisconsin Collaborative for Healthcare Quality (WCHQ) – a voluntary association of provider groups and health systems across Wisconsin that develop, collect, and report data on their performance measures. UW Health has been reporting CRC screening data since 2005. In 2008, we were surprised to find that we were not among the top health systems in Wisconsin with respect to our CRC screening rates, which was around 61% at the that time. We were above the national average, but our leaders knew we could do better and made it a strategic priority to increase UW Health CRC screening rates. To address this priority, the UW Health Colorectal Cancer Prevention Initiative (CCPI) was formed. CCPI is a multidisciplinary group with members from primary care, gastroenterology, radiology, quality improvement, clinic management, and academic research with the main goal of making CRC screening easier, more accessible, and more appealing for patients and providers.
What did you learn about screening variation among providers?
The first step of CCPI was to determine our current CRC screening rates and practices. We decided to dive deeper and examine the degree of variation in CRC screening rates within our system. We found that there was substantial variation across primary care clinics (range of 42-80% CRC screening rates), as well as between primary care providers within the same clinics (range 38-87% CRC screening rates). Unintended variation can undermine the quality of care we deliver to our patients, so we administered a survey to all UW Health primary care providers to help understand the variation in CRC screening rates. We were able to identify predictors of CRC screening variation at multiple levels of the healthcare system (patient, provider, and healthcare organization) and concluded that interventions to increase CRC screening rates need to be directed at all levels of the system.
What were your next steps?
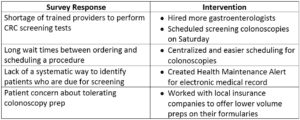
The primary care provider survey included questions about CRC screening barriers at the patient, provider, and system levels. We used the survey results to design and implement interventions to directly address these barriers (some examples are listed below):
We are happy to report that through the hard work of the CCPI, we have seen an increase in UW Health’s CRC screening rates from 61% to 81% and the 81% has been sustained over the past three years. Our next steps are to further evaluate the interventions that were implemented and determine which ones gave us the “biggest bang for the buck”.
What lessons learned would you share with others that are working to increase colorectal cancer screening in primary care settings?
The most important lessons that we learned are:
- Start by gathering your data and design a process for continual assessment
- Have buy-in from institutional leaders
- Organize the process to increase CRC screening from the start
- Target multiple levels of the healthcare system: patients, providers, and the healthcare organization
Were there tools, trainings or resources that you found helpful?
Our first step was to learn best practices from successful health systems in Wisconsin and start conversations about the lessons they learned on their journey to increase CRC screening rates. The NCCRT tool, “How to Increase Colorectal Cancer Screening Rates in Practice: A Primary Care Clinician’s Evidence-Based Toolbox and Guide” is a fantastic resource with many relevant and useful templates that can easily be incorporated into practice.
Do you have any final tips for our readers that are working to achieve 80% by 2018?
Start by gathering the necessary people for your team, which can be patients, providers, clinic staff, and system administrators. Next, identify current barriers to reaching this goal and let them inform your interventions. Finally, a strong commitment to this goal is necessary. It can be done and you may even surprise yourselves and reach 80% before 2018!
Thank you for sharing your story with us! We look forward to hearing more about your work and UW Health’s journey in the future.

[vc_widget_sidebar sidebar_id=”sidebar-1″]
"*" indicates required fields


