Interview with C. L. Brumback Primary Care Clinics—80% by 2018 National Achievement Award Honoree

April 17th, 2017 :: Author: Belma Andrić, MD, MPH
On February 1, 2017, C. L. Brumback Primary Care Clinics became an Honoree recipient of the 2017 80% by 2018 National Achievement Awards, a program designed to recognize individuals and organizations who are dedicating their time, talent and expertise to advancing needed initiatives that support the shared goal to regularly screen 80% of adults 50 and over by 2018.
Belma Andrić, MD, MPH is the Chief Medical Officer of the Health Care District of Palm Beach County. Dr. Andric is responsible for quality and patient safety across the Health Care District and directly supervises the Trauma, Aeromedical and Quality and Patient Safety departments, with indirect oversight over the District’s other physician leaders. Previously Dr. Andric has served as the Medical Director of the Health Care District’s C. L. Brumback Primary Care Clinics that serve over 30,000 unduplicated patients annually. She was in charge of quality and clinical performances at eight clinics locations.
Hi, Dr. Andrić! We’re excited to feature your work on the 80% by 2018 Blog. Can you tell us a little about yourself and how you ended up working on colorectal cancer screening?
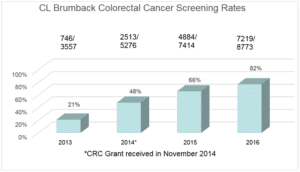
I have worked as a medical director with C. L. Brumback Primary Care Clinics since their founding as a federally qualified health center (FQHC) in 2013. Early on, we realized we needed to work on establishing solid clinical preventive services to improve the health of all our patients. We adopted “an ounce of prevention is worth a pound of cure” as part of our mission. We also knew our efforts would require widespread application of primary and secondary prevention guidelines, as well as intensive data collection, analysis, feedback and ongoing quality improvement (QI) initiatives. Not to mention, being a new FQHC, we had to work to improve many quality indicators simultaneously. With all this, a realization set in that an ounce of prevention is a ton of work. To overcome these challenges, we formed separate working groups for different QI initiatives, including one with a goal to improve our colorectal cancer (CRC) screening rates. This group began by looking for best practices among peer clinicians and staff. We also applied for a CHANGE grant from the American Cancer Society to provide more resources for a project focused on CRC screening. We received the award at the end of 2014, and that was the beginning of our successful journey on the road to reach our goal of 80% by 2018.
Tell us a little bit about C. L. Brumback Primary Care Clinics.
The C. L. Brumback Primary Care Clinics strive to provide the highest quality health care to all Palm Beach County residents, including the homeless and migrant populations. In just a few years, we went from serving 13,000 unduplicated patients in 2013 to over 35,000 in 2016. Currently, we provide adult medical, pediatric, dental and women’s health services at nine different clinic locations. We are scheduled to open two new clinic locations in underserved areas of our county in 2017. But as our Executive Director Mr. Christopher Irizarry often says, “What we are most proud of is not the number of patients we have served, but the fact that as our volume and sites increased, so did the quality of care to our patients!”

When and why did C. L. Brumback Primary Care Clinics decide to focus on increasing colorectal cancer screening?
Our CRC screening rate in 2013 was 21%. It was a “no brainer” that something needed to be done, but where to start? Our small QI department started meeting regularly to brainstorm about possible CRC screening interventions. During these meetings, we decided to apply for the CHANGE grant, and that was the “game changer” for us. Once we received the award, we started working closely with our local ACS liaison, Jennifer Bustamante, Florida’s primary care health systems manager, to understand what strategies work in community health centers like ours.
What activities and systems changes did you implement, and how did you choose them?
Early on we learned the power of patient navigation, so as a first step we hired a patient navigator. And we did not go far away for that: we promoted one of our front-line registrars since we needed someone who knew our patients and knew the “beat” of the clinics. This proved to be one of the best decisions we made. The patient navigator completely owned the program. Her success was built on her knowledge of clinic procedures and work flows, as well as being able to establish trusting relationships with patients. Our patient navigator also navigates all of us toward mutual goals. She organizes “lunch and learn” meetings dedicated to CRC screenings, runs weekly/monthly reports that keep us up to date on how we are doing, leads process improvements, develops tools, etc.
Next, we started by identifying barriers to screening among the unscreened and learned a top barrier is that their doctors did not tell them they needed to be screened. So we worked hard to create a culture in which we always “think CRC screening.” In our clinics, patients are offered screening at each visit regardless of the reason for their visit. Today, in our clinics, patients can expect they will be offered CRC screening the same way they expect their blood pressure would be checked. In other words, it’s become second nature. We implemented numerous interventions, including care team education and training, optimized clinic flows, morning huddles and monthly staff meetings focused on CRC screening, standing orders for MAs and providers, optimized EHR documentation and data collection, and transparent sharing with providers on where we stand regarding CRC screening rates. Know your numbers became our new mantra; each month we share our current rates as a group and for individual teams. We celebrate our success and identify champions, and we create healthy competitions among care teams (hint: doctors are very competitive! J) As a result, we’ve seen steady rate improvements month after month.
I understand you piloted a strategy you call “poop on demand.” What is this?
During “lunch and learn” meetings, we share best practices between clinics and adopt innovative ideas that staff share. A great example of thinking out of the box came from one of our nurses: instead of giving FIT tests to patients to take  home with them, politely and a bit humorously, we simply ask patients to try to use clinic restrooms and collect their stool specimen during that visit. And to our surprise, many patients cooperated! So we incorporated this into our FIT test guidance for medical assistant and nurses and adopted it across the board. This increased our overall FIT test compliance rates by 30-40%. We called it “poop on demand” – a tool with a funny name but powerful results. We also discovered that some FIT tests were unsatisfactory upon return due to too little or too much (leaking kits) stool in the specimen, so we developed “stool models” out of Play-Doh for medical assistants to demonstrate proper stool collection.
home with them, politely and a bit humorously, we simply ask patients to try to use clinic restrooms and collect their stool specimen during that visit. And to our surprise, many patients cooperated! So we incorporated this into our FIT test guidance for medical assistant and nurses and adopted it across the board. This increased our overall FIT test compliance rates by 30-40%. We called it “poop on demand” – a tool with a funny name but powerful results. We also discovered that some FIT tests were unsatisfactory upon return due to too little or too much (leaking kits) stool in the specimen, so we developed “stool models” out of Play-Doh for medical assistants to demonstrate proper stool collection.
What success have you seen? How did you measure that success?
As a direct result of all these interventions, we’ve seen a four-fold increase in our screening rates in three years, at the same time that our denominator (number of patients eligible for screening) doubled. This also means we are removing more and more precancerous polyps. To date we have diagnosed two patients with CRC after routine screening. These results are powerful motivational tools for all of us in community health centers since it is proof that CRC screening programs not only detect cancers early in people who do not have obvious symptoms but also prevent cancer from ever developing. It is also especially motivational for us since we serve as a safety network for patients with limited resources and who would otherwise not have access to screening.
What lessons learned would you share with others that are working to increase colorectal cancer screening in primary care settings?
Don’t get discouraged by road blocks, especially in community health centers settings. Some road blocks we could anticipate, and some we could not. Most of the issues we identified and resolved “on the run” as we learned them. For example, we knew early on that we needed to find a colonoscopist who would be willing to see uninsured patients who tested positive with the FIT test. Fortunately, we found a partner at a local community hospital; however, that hospital is located in a rural area 40-50 miles away from our closest clinic location and travel requires three to four bus lines with a travel time of two hours in each direction. From NCCRT’s resource, Steps for Increasing Colorectal Cancer Screening Rates: A Manual for Community Health Centers, we learned about the concept of open access colonoscopy, so we started to educate patients on  bowel prep so that they could make the trip only once – on the day of the procedure. We trained the
bowel prep so that they could make the trip only once – on the day of the procedure. We trained the
nurses on the bowel prep procedures and developed patient instructions, as well as standing orders for colonoscopy prep for providers. One of the unanticipated problems was poor prep. Luckily, our very first patient’s prep was inadequate, so we learned this valuable lesson early on and added additional layers of patient navigation. On the day of bowel prep, patient navigators call the patient up to a few times to ensure good understanding and compliance with instructions. We simply could not waste a valuable colonoscopy spot to poor bowel prep. As a result, the more than 80 colonoscopies conducted in the next 18 months had excellent prep, and we’ve seen 100% compliance with transportation that’s arranged by the patients themselves.
Were there tools, trainings or resources that you found helpful?
Early on, NCCRT’s guide, Steps for Increasing Colorectal Cancer Screening Rates: A Manual for Community Health Centers, became an indispensable resource in our work. Currently, one of the most important tools we’re using is our population management platform. This platform gives us the capacity to analyze data down to the physician and patient level and provides us performance feedback and comparative benchmarking information. In my opinion, this very user-friendly, close-to-real-time physician-level reporting is the most important tool for program sustainability. This make us all “own it” and be responsible for the population we serve.
Do you have any final tips for our readers that are working to achieve 80% by 2018?
“The healthcare provider never suggested I get this test” has been cited as the primary barrier to CRC screening among those who have never screened or are overdue for screening. This is the reason we focus on training our staff on the importance of CRC screening as well as putting the systems in place to make screening an easy choice for patients in all our clinics. We found that once we put our act together, patients trusted us and complied with recommended screening recommendations. We led them, and they followed us.
Thank you for sharing your story with us! We look forward to hearing more about your work and C. L. Brumback Primary Care Clinics’ progress in the future.

We Highlight Successes, Leaders, Best Practices, And Tools That Are Making An Impact In The Nationwide Movement To Reach 80% Screened For Colorectal Cancer.
Do you have a suggestion for a future blog topic? We welcome you to share your suggestions by emailing [email protected].
Blog Policy
Opinions expressed in these blog posts are that of the author and do not represent policies of the National Colorectal Cancer Roundtable or the author’s institution.
Our staff moderate all comments on the 80% Blog. While we do not censor based on point of view, we will delete or edit comments that are offensive or off topic. Click here to view full version.
© 2024 American Cancer Society National Colorectal Cancer Roundtable. All rights reserved.


