Intervention Type: Provider Assessment & Feedback

Blue Star Conversations – September 11, 2023
Steps for Increasing Colorectal Cancer Screening Rates: A Manual for Primary Care Practices

Blue Star Conversation – May 17, 2023
Meeting Summary – Primary Care Strategy Meeting: Catalyzing Primary Care to Increase Colorectal Cancer Screening

Webinar: 2022 NCCRT Steps Guide Update – July 25, 2022
How Can Women’s Health Providers Save More Lives from Colorectal Cancer?
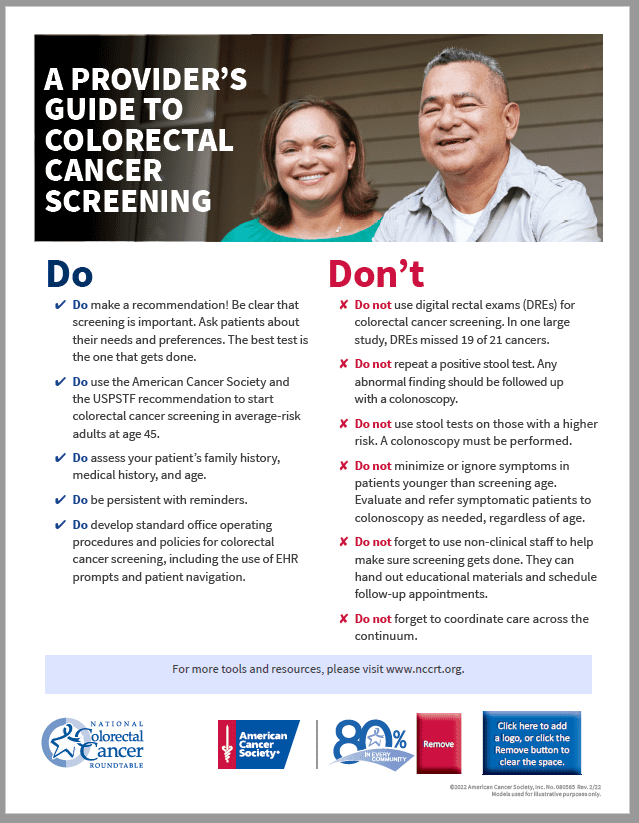
The Dos and Don’ts of Colorectal Cancer Screening
NCCRT Learning Center